MBL epidemiology
Metallo-β-lactamase-producing pathogens may be an increasing and substantial threat for your patients1,2
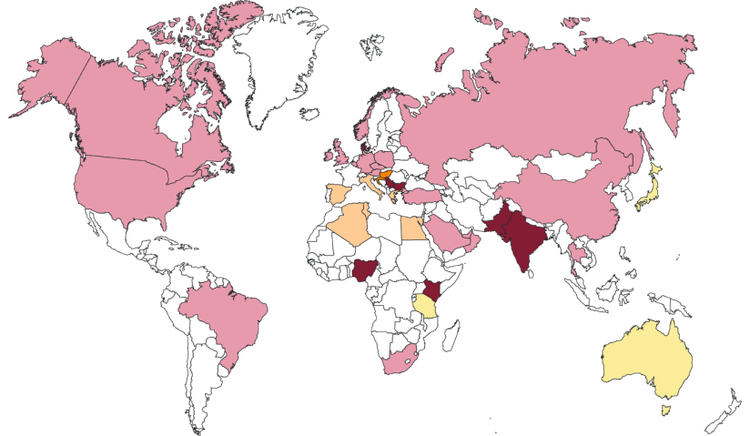
Metallo-β-lactamase (MBL)-producing bacteria are on the rise.1 Their epidemiology is global, and they are spreading, representing a significant challenge for clinical management and public health.1,2
Most prevalent carbapenemase in the country
-

-

-

-

Most prevalent MBL group in countries where serine carbapenemases (KPC or OXA-48-like) are more prevalent
-

-

-

-

The COVID-19 pandemic saw an increase in infections caused by MBL-producing pathogens, contributing to antimicrobial resistance (AMR).3–5
Results from the Global Antimicrobial Resistance and Use Surveillance System (GLASS) Report on the impacts of COVID-19 on AMR show that there was an:4
- Increase in AMR among Gram-negative organisms (Klebsiella pneumoniae, Acinetobacter spp. and Escherichia coli)
- Increase in total prescribing of antibiotics, especially in low-to-middle income countries
Bacteria with NDM, VIM and IMP enzymes have been identified in community, hospital and environmental settings throughout the world.1
- The highest prevalence of NDM-producing Enterobacterales are found in the Indian subcontinent, parts of Asia-Pacific, the Middle East and southeast/eastern Europe6,7
- VIM-producing Enterobacterales are common in parts of southeast Europe6,7
- IMP-producing organisms are mainly found in Japan, China and Australia6,7
- With the exception of Antarctica, IMP, VIM and NDM enzymes have successfully spread to all continents since they were first detected in 1991, 1997 and 2008, respectively2,8
- With the increasing epidemiology, no part of the world is immune to antimicrobial resistance problems caused by MBL-producing pathogens1,6,7
- India faces a significant challenge with AMR, especially with Gram-negative bacteria that are resistant to Carbapenems. According to an Indian study, MBL was identified in 48% of the Carbapenem-resistant K. pneumoniae isolates and 76% of Carbapenem-resistant E. coli.16
What has been happening in India at a national level?
The incidence of carbapenemases in India over time9
Carbapenemase trend over the years among overall CRE from ICU settings including CR-E.coli and CR-Klebsiella spp.
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| Total Enterobacterales | #FEEA31 | 241 | 329 | 578 | 552 | 568 |
| CRE | #94C201 | 77 | 122 | 229 | 229 | 234 |
| NDM | #0095FF | 35 | 80 | 155 | 137 | 174 |
| OXA-48 | #0DBDBA | 38 | 75 | 148 | 156 | 141 |
| KPC | #F49C34 | 0 | 0 | 4 | 1 | 0 |
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| Total Enterobacterales | #FEEA31 | 241 | 329 | 578 | 552 | 568 |
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| CRE | #94C201 | 77 | 122 | 229 | 229 | 234 |
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| NDM | #0095FF | 35 | 80 | 155 | 137 | 174 |
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| OXA-48 | #0DBDBA | 38 | 75 | 148 | 156 | 141 |
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| KPC | #F49C34 | 0 | 0 | 4 | 1 | 0 |
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| Total E.coli | #FEEA31 | 81 | 85 | 179 | 178 | 195 |
| CR-E.coli | #94C201 | 15 | 17 | 39 | 45 | 48 |
| NDM | #0095FF | 11 | 16 | 36 | 41 | 48 |
| OXA-48 | #0DBDBA | 2 | 2 | 10 | 5 | 6 |
| KPC | #F49C34 | 0 | 0 | 0 | 0 | 0 |
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| Total E.coli | #FEEA31 | 81 | 85 | 179 | 178 | 195 |
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| CR-E.coli | #94C201 | 15 | 17 | 39 | 45 | 48 |
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| NDM | #0095FF | 11 | 16 | 36 | 41 | 48 |
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| KPC | #0DBDBA | 2 | 2 | 10 | 5 | 6 |
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| OXA-48 | #F49C34 | 0 | 0 | 0 | 0 | 0 |
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| Total Klebsiella | #FEEA31 | 100 | 155 | 285 | 278 | 291 |
| CR- Klebsiella spp. | #94C201 | 56 | 88 | 161 | 163 | 175 |
| NDM | #0095FF | 22 | 47 | 94 | 80 | 116 |
| OXA-48 | #0DBDBA | 36 | 64 | 133 | 140 | 132 |
| KPC | #F49C34 | 0 | 0 | 2 | 1 | 0 |
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| Total Klebsiella spp. | #FEEA31 | 100 | 155 | 285 | 278 | 291 |
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| CR- Klebsiella spp. | #94C201 | 56 | 88 | 161 | 163 | 175 |
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| NDM | #0095FF | 22 | 47 | 94 | 80 | 116 |
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| OXA-48 | #0DBDBA | 36 | 64 | 133 | 140 | 132 |
Incidence of carbapenemases in Enterobacterales from 2018 to 2022
| No. of confirmed carbapenemases | 2018 | 2019 | 2020 | 2021 | 2022 | |
| KPC | #F49C34 | 0 | 0 | 2 | 1 | 0 |
The Burden
Infections caused by MBL-producing Enterobacterales cause higher mortality rates compared to non-carbapenemase producing CRE10–13
Explore in detail the burden of MBL-producing Enterobacterales on patient outcomes.

Understanding MBLs
Did you know that MBLs account for the majority of the ‘Big Five’ carbapenemases?14,15
Discover more about the ‘Big Five’ carbapenemases, including MBLs.
- Boyd SE, et al. Antimicrob Agents Chemother 2020;64:e00397-20.
- Wu W, et al. Clin Microbiol Rev 2019;32:e00115-18.
- Mojica MF, et al. Lancet Infect Dis 2022;22(1):e28–e34.
- Tomczyk S, et al. J Antimicrob Chemother 2021;76(11):3045–58.
- Ayoub Moubareck C, et al. Front Cell Infect Microbiol 2022;12:823626.
- Sader HS, et al. J Antimicrob Chemother 2021;76:659–66.
- Sader HS, et al. Eur J Clin Microbiol Infect Dis 2022;41:477–87.
- Meletis G. T her Adv Infect Dis 2016;3:15–21.
- Abstracts at CIDSCON 2024. Journal of Clinical Infectious Diseases Society 2(3):p 163-292, Jul–Sep 2024. | DOI:10.4103/CIDS.CIDS_56_24
- Tamma PD, et al. Clin Infect Dis 2017;64:257–64.
- de Jager P, et al. PLoS One 2015;10:e0123337.
- Daikos GL, et al. Antimicrob Agents Chemother 2009;53:1868–73.
- Hayakawa K, et al. J Antimicrob Chemother 2020;75:697–708.
- Henderson J, et al. J Hosp Infect 2020;104:12–19.
- Bonnin RA, et al. Front Med (Lausanne) 2021;7:616490.
- Bakthavatchalam YD et al .In vitro activity of ceftazidime-avibactam and its comparators against carbapenem resistant Enterobacterales collected across India: results from ATLAS surveillance 2018 to 2019. Microbiol Infect Dis. 2022;103:115652.